Individual and Family
Understand Your Health Insurance Plan: What Is an In-Network Provider?
Published on July 10, 2024
Share
- Cost Savings: Utilizing in-network providers reduces your out-of-pocket healthcare costs due to pre-negotiated rates.
- Better Coverage: In-network providers offer greater coverage benefits, reducing how much you pay for medical services.
- Easier Billing: In-network providers handle billing directly with your insurance, simplifying the claims process for you.
What are provider networks?
If your plan requires or prefers you to use in-network health care providers, you probably want to know what this means in the first place.
A provider network is a group of physicians and specialists of health-care providers who are contracted by an insurance company, and provide medical care to those enrolled in plans offered by that insurance company. The providers in the health insurance plan’s network are called “network providers” or “in-network providers”. This term could apply to doctors, medical facilities, and other types of health-care providers.
Why do health insurance plans have provider networks?
Many health insurance plan types cut costs for their enrollees by having their networks full of in-network providers, according to America’s Health Insurance Plans (AHIP). These providers charge lower rates in exchange for being part of the provider network of a given insurance company.
Health insurance plans that have in-network providers are referred to as “managed-care” plans. This model has become increasingly popular, with the market now dominated by plans with a list of doctors and facilities for enrollees to choose from.
What is an In-Network Provider?
When it comes to understanding your health insurance, it’s important to know the difference between in-network vs. out-of-network. A provider network is a directory of hospitals, doctors, and other healthcare providers who have contracted with a particular health care plan to provide services for its members. What is an in-network provider? An in-network provider is a healthcare professional or facility that is part of an insurance company’s network, offering services at negotiated rates to plan members.
Out-of-network providers are different from in-network providers, as out-of-network providers have not agreed to accept pre-determined payment amounts, and they will likely charge more than in-network providers. Despite this fact, the insurance plan may not always pay the higher costs, as they’re not required to. If the health insurance plan only agrees to pay the rate for in-network providers and you have seen an out-of-network provider, then you will be responsible for paying the difference. The provider will bill you after the health insurance plan has declined to pay the billed amount in full.
Benefits of using In-Network Providers vs. Out-of-Network
Choosing between in-network and out-of-network providers can significantly impact both your healthcare experience and expenses. In-network providers are contracted with your health insurance plan to offer services at lower negotiated rates, typically leading to cost savings and smoother billing processes for you. Conversely, out-of-network providers do not have such agreements with your insurance, which can result in higher costs and additional paperwork. Understanding the benefits and drawbacks of each can help you make informed decisions that optimize your healthcare benefits while managing costs effectively.
Cost savings
One of the significant benefits of choosing in-network providers is cost savings. In-network providers have agreements with your health insurance company to offer services at discounted rates, which are pre-negotiated to be lower than what you might typically pay. This arrangement means that when you opt for in-network care, your out-of-pocket expenses are generally reduced, making it a financially smarter option for routine care and unexpected medical needs alike. By leveraging these negotiated rates, you ensure that your healthcare dollars go further while still receiving quality care.
To provide a better understanding of in-network vs out-of-network costs, here is a table that can help you with specific figures as an example:
| In-Network Hospital – pays 80% | Out-of-Network Hospital – pays 60% | |
| Actual hospital charge | $22,000 | $22,000 |
| Amount hospital agrees to pay | $14,000 (this is the agreed upon discounted rate) | $14,000 (this plan does not agree to pay the $8,000 difference |
| Medical plan pays | 80% of the discounted rate:$14,000 x 80% = $11,200 | $14,000 x 60% = $8,400 |
| Covered individual pays: | 20% of the discounted rate:$14,000 x 20% = $2,800 | 40% of charges ($14,000) in addition to all of the amount that the plan does not agree to pay ($8,000):$5,600 + $8,000 = $13,600 |
As you can see, there can be significant differences in the costs involved with an in network provider as opposed to an out-of-network provider. Of course, this will depend on the specific healthcare facility, as well as the service provided, but you will typically pay less with an in-network provider.
Simplified billing
Using in-network providers significantly simplifies the billing process for healthcare services. These providers have established agreements with your insurance company, allowing them to bill the insurer directly for the services you receive. This direct billing method not only streamlines transactions but also significantly reduces the amount of paperwork and administrative tasks you need to handle. As a result, you can focus more on your healthcare and less on the complexities of filing claims and managing out-of-pocket expenses, making the overall experience more convenient and hassle-free.
Quality assurance
Using in-network providers also offers a level of quality assurance that can be beneficial for patients. Insurance companies typically vet the providers within their networks, ensuring they meet specific standards of care and professional qualifications before they are included. This vetting process helps maintain a high standard of healthcare quality for insured individuals. Additionally, being within an insurance network often grants patients access to a comprehensive range of services and specialists, enhancing the likelihood of receiving coordinated and thorough care. This broad access ensures that you can find the right specialists and services within the network, facilitating better health outcomes and continuity of care.
Plan types that use In-Network Providers
The use of in-network providers impacts different types of health insurance plans, including Preferred Provider Organizations (PPOs), Health Maintenance Organizations (HMOs), Point of Service (POS) plans, and Exclusive Provider Organizations (EPOs).
Keep in mind that each plan has its own terms and limitations, so be sure to check the official plan documents to understand how that specific plan works.
Preferred Provider Organization (PPO)
As the name suggests, PPOs have preferred providers that have been selected for your use. While the insurance company does prefer you use their chosen, in-network providers, there is some flexibility with going out-of-network—it just may mean the insurance company covers less of the care rendered outside of the network.
Health Maintenance Organization (HMO)
With this type of plan, you will likely be more limited to the provider network of the HMO, and you will most likely need to choose a primary care physician (PCP) for all referrals. HMOs usually have lower premiums than other plan types, such as PPOs.
Point of Service (POS)
Think of POS plans as a hybrid of HMO and PPO plans. You will likely have to choose a PCP within the health insurance plan’s network, but as with a PPO, you have the flexibility to go to out-of-network providers, perhaps just at a higher cost.
Exclusive Provider Organizations (EPOs)
Exclusive Provider Organizations (EPOs) offer a distinct model within the health insurance landscape, blending aspects of various plan types but with specific limitations and advantages:
- In-Network Provider Requirement: EPOs require you to use doctors, specialists, and hospitals within the plan’s network except in emergency situations. This network restriction helps keep the costs under control, as all non-emergency services must be obtained from providers who have agreed to lower their rates for plan members.
- Potential for Lower Premiums: Compared to Preferred Provider Organizations (PPOs), EPOs often feature lower premiums. This cost-saving benefit arises because EPOs limit member access to a defined network of providers and do not cover out-of-network care except in emergencies, thereby reducing the insurance company’s overall expenses.
These characteristics make EPOs a suitable choice for individuals who are looking for more affordable insurance options and are comfortable with the limited choice of providers in exchange for lower monthly premiums.
How to find In-Network Providers
eHealth has convenient tools that you can use if you are shopping for a plan and want to figure out who is in that plan’s network. This may be important to you if you already have a doctor in mind who you want as your primary care provider (PCP).
Whether you have individual health insurance or a group health plan, you can use our Find a Doctor tool to get started on looking at plans that have certain doctors in-network.
Each insurance plan periodically updates its list of in-network doctors and providers, so always double check coverage with both the plan and the doctor or provider before incurring medical expenses. You can also figure out who is in your network by directly contacting your provider or checking your insurance company’s website.
Find a health insurance provider that’s right for you
As you can see, there are some advantages to choosing an in-network provider, but who you see for your health concerns is ultimately up to you. If you need help figuring out a health insurance plan that is within your reach, you can use eHealth. Our team of licensed agents are available to help you find a health insurance plan that’s right for your specific needs. Contact us today and our agents will connect you with health insurance providers who will help you manage getting the medical care you need.
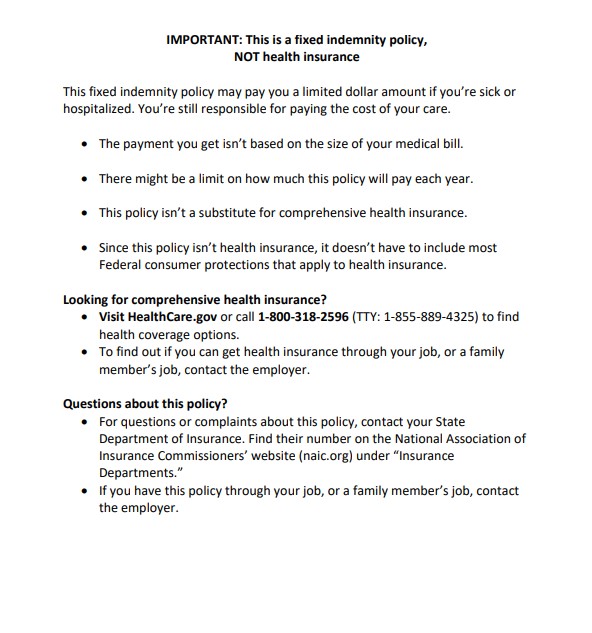
Choosing a plan is different for everyone. The amount of in-network providers, and the flexibility to go out of network may be hugely important to some people buying a health insurance plan. Luckily, when shopping on eHealth, you will get the information you need in order to make an informed decision about which managed-care plan you want to choose for your health insurance coverage. And if you decide that in-network providers and managed care aren’t for you, we have just as many resources when it comes to health insurance alternatives, like medical indemnity insurance.